Personalizing Your RA Treatment: 5 Questions to Ask Your Doctor - CreakyJoints
Wouldn't it be great if you could find out which exact drug will work best for your rheumatoid arthritis (RA) before you take it? Fortunately, scientists are working hard to develop tests to provide this type of precise information — but for now, the typical RA treatment course entails quite a bit of trial and error. Patients are often required to test out medication after medication before finding one that controls their disease without causing too many side effects.
Additionally, while the wide array of RA drugs on the market today is a mostly a good thing, the sheer number of available options means it can be hard to know where to start or what your next move should be. Will a conventional disease-modifying anti-rheumatic drug (DMARD) like methotrexate be sufficient? Will you respond to a tumor necrosis factor (TNF) inhibitor like infliximab (Remicade)? Or is a Janus kinase (JAK) inhibitor like tofacitinib (Xeljanz) a better fit for you? And what about other DMARDs that act on other parts of your immune system, like abatacept (Orencia), rituximab (Rituxan), and anakinra (Kineret)?
If you're worried that your doctor may have prescribed a treatment that will not work for you, take heed: While precision medicine for RA is still in its infancy, rheumatologists aren't blindly guessing, either. Instead, they're making informed choices that factor in clinical practice guidelines, your personal health history, and other factors.
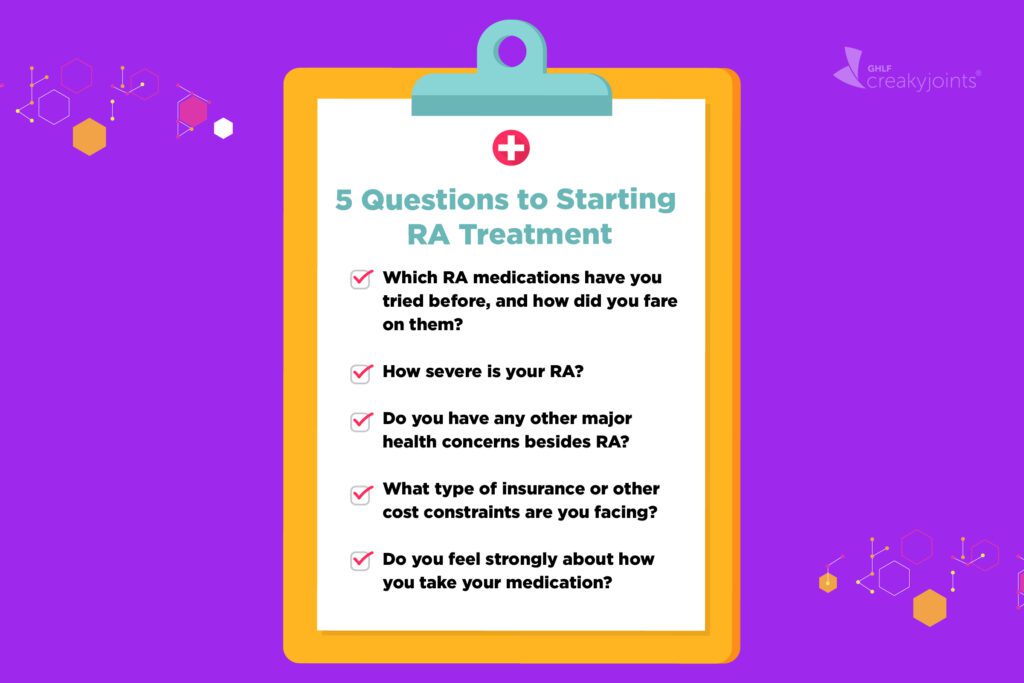
Considering the following five questions before trying any new treatment can help get you and your rheumatologist get to the right medication faster.
1. Which RA medications have you tried before, and how did you fare on them?
If you've just been diagnosed with RA, chances are your doctor will start you on methotrexate. The American College of Rheumatology (ACR) recommends it as the first-line treatment, because it tends to work relatively quickly, is inexpensive, and has a long track record of efficacy.
If you can't take methotrexate — or if your disease has not been sufficiently controlled on it — then the ACR advises using a biologic DMARD in the tumor necrosis factor (TNF) inhibitor class. These drugs work very well for some people, but about half of RA patients that try them don't respond to them, probably because their RA is not being primarily driven by TNF but instead by another inflammatory cytokine (protein).
Many patients just start a TNF inhibitor and see what happens, but if it doesn't work, you risk having your disease progress. Instead, this might be a good opportunity to ask your doctor about PrismRA, a blood test that combines a biomarker panel with a machine learning-based algorithm, says J. Eugene Huffstutter, MD, a rheumatologist with Arthritis Associates in Hixson, TN. Research has shown that PrismRA can predict with 90 percent accuracy who will not respond to a TNF inhibitor with a test result of inadequate response.
If you've previously tried at least one TNF inhibitor and it hasn't worked, or if you've taken the PrismRA test and it identified you as a non-responder, then you're likely better off moving to a drug in a different class instead of experimenting with a second or third TNF inhibitor, says rheumatologist Isabelle Amigues, MD, assistant professor at National Jewish Health in Denver, CO. Instead, ask your doctor if you're a good candidate for a different type of DMARD.
2. How severe is your RA?
Some people's RA is mild and it stays that way, whereas others have high disease activity that's hard to control. It's not always possible to predict which way you'll ultimately go, but rheumatologists do have some clues to go on.
"If a patient already has erosion that's visible on X-rays and is positive for CCP and RF [autoantibodies that indicate your body is attacking its own tissue], we know they're most likely to need aggressive treatment soon," says Amigues.
In such patients, "The goal is to get them into remission quickly, because the earlier you get them into remission, the longer they'll stay in remission" and less permanent damage will be done, she says.
3. Do you have any other major health concerns besides RA?
When it comes to choosing the right drug — as well as avoiding a potentially dangerous one — it's very important to pay attention to comorbidities, which are other conditions or life plans that you might have in addition to RA. For example, if you are of child-bearing age and planning to have a child soon or are pregnant, it is important to avoid methotrexate and leflunomide during this time.
4. What type of insurance or other cost constraints are you facing?
In a perfect world, you and your doctor will have total control over which medication to use, but that's not usually how it works. In reality, your health insurance provider will probably limit your options in some way. They might refuse to pay for any biologic medication unless you first go through an appeals process, or they might require you to try and fail one or several TNF inhibitors before agreeing to pay for a drug in a different class.
The problem is that biologics are quite expensive, and insurers have contracts with pharmaceutical companies that make certain drugs more cost-effective for them than others — at least in the short term.
Of course, if a patient doesn't respond to a given medication, their disease might escalate, which can lead to much bigger expenditures (surgeries, hospitalizations, etc.) down the line. "Insurance companies aren't looking at the long-term; they're looking year to year or even quarter to quarter," says Huffstutter.
If cost is of top concern — perhaps your co-payments are high or you're paying for everything out of pocket — you should also know that triple therapy (using three traditional DMARDs together) is significantly less expensive than taking methotrexate plus a TNF biologic, yet research suggests this older option often works equally well.
6. Do you feel strongly about how you take your medication?
All TNF inhibitors are taken at home by self-injection or infusion. While some people find that going for infusions is terribly inconvenient, others hate giving themselves shots so much that they'd rather leave medication administration to the professionals.
If you're only willing to take medication orally, you still have options: Conventional DMARDs like methotrexate and targeted synthetic DMARDs like the JAK inhibitor tofacitinib come in pill form.
Of course, the best drug for you is the one that works, but personal preference also matters, so be sure to discuss any concerns you might have with your doctor. "Never be afraid to speak up — because this is the person with the degree and I'm just the patient," says rheumatologist Grace C. Wright, MD, PhD, Founder and President of the Association of Women in Rheumatology (AWIR). "No, you're the person living in the experience, I'm here to serve you."
This article is part of "Your Guide to Precision and Personalized Medicine for Rheumatoid Arthritis" and was made possible with support from Scipher Medicine.
- Was This Helpful?

Comments
Post a Comment