A systematic review and meta-analysis protocol for insomnia | JPR - Dove Medical Press
Introduction
Insomnia is a common clinical condition that occurs independent of or comorbid with other physical or psychological diseases.1 An estimated 50% of adults suffer from insomnia symptoms each year, 15% experience chronic symptoms,2 and lifetime prevalence estimates indicate that on average ~10% of the population meet the diagnostic criteria of insomnia disorder.3–5 Prevalence estimates vary depending on age, assessment tools, and the criteria applied. Using stringent DSM-IV diagnostic criteria, point prevalence estimates in a large sample remained 6%,6 whereas a recent cross-cultural and comparative epidemiological study reported that 10.8% fulfilled the newer DSM-5 criteria for insomnia disorder.7 In a recent meta-analysis, the pooled prevalence of insomnia disorder in China was 15.0%.8 Regardless of the population and instruments used, insomnia is common.
Insomnia can affect people of all ages, especially older adults (>65 years), women, smokers, and overweight individuals.9 Patients with insomnia often complain of reduced sleep and/or quality of sleep that seriously affects their quality of life and social functioning during the daytime, especially through sleepiness, fatigue, malaise, mood lability, attention/concentration/memory impairment, productivity decline, work absenteeism, and even road traffic accidents.1,10 Furthermore, persistent sleeplessness is associated with a higher risk of diabetes,11 Alzheimer's disease,12 psychological disorders,13,14 and cardiovascular disease,15,16 which might aggravate co-morbidities and suicidal thoughts.17,18 Thus, patients should be aware of insomnia and be actively treated, while physicians should pay attention to the sleep quality of their patients who may have comorbid insomnia despite visiting for other reasons.
The management of insomnia currently relies on both pharmacological and non-pharmacological therapies.19–21 Benzodiazepines and non-benzodiazepine hypnotics are frequently used to manage insomnia and promote sedation by enhancing gamma-aminobutyric acid (GABA) function in the brain.22 In most guidelines, due to the potential risks of tolerance and reliance, hypnotic medications are only advised for short-term use (maximum 4 weeks).19–21 Antidepressants have also widely been adopted to improve insomnia, especially in people with concomitant conditions such as chronic pain and depression, despite being off-label for insomnia and lacking sufficient evidence.23 In addition, as a new kind of hypnotic, suvorexant has the potential to shorten sleep latency and lengthen total sleep time by antagonizing orexin receptors.24 However, these hypnotic drugs and antidepressants give rise to some serious adverse reactions including hangover, parasomnias, sleep paralysis, memory problems, arrhythmia, falls, headache, nausea, fatigue, and rebound insomnia.19–24 As a result, non-pharmacological interventions are the preferred treatment for insomnia. First-line treatment is cognitive behavioral therapy for insomnia (CBT-I), which has been proven to be highly effective and is recommended globally.19–21,25 Nevertheless, CBT-I has some limitations. First, some CBT-I techniques place high demands on patients through sleep restriction, stimuli control, and cognitive restructuring, resulting in poor adherence.26,27 Secondly, the high cost of treatment and the lack of behavioral sleep medicine specialists restrict access of CBT-I to many patients.26,27 Third, CBT-I is ineffective in 20–30% of insomnia patients.28 Therefore, other non-pharmacological alternatives are required to help more patients with insomnia.
Since ancient times, the Chinese healthcare system has made extensive use of acupoint stimulation-related therapies (ASRTs), which are based on the meridian theory of traditional Chinese medicine (TCM). ASRTs describe methods of preventing and treating diseases by stimulating particular places on the body (called acupoints) with various needles or other non-needle techniques and manipulations. Recently, an increasing number of randomized controlled trials (RCT) have demonstrated that manual acupuncture (MA),29,30 electroacupuncture (EA),31,32 laser acupuncture,33 acupoint catgut embedding (ACE),34 acupressure,35 moxibustion,36 and transcutaneous electrical acupoint stimulation (TEAS)37 can improve the sleep quality of patients with primary insomnia without serious adverse effects, with EA even safe for use in pregnant women with insomnia.38 In addition, individuals with comorbid insomnia are increasingly using these common clinical ASRTs, and several RCTs have reported positive outcomes for the management of insomnia with EA and MA in patients with stroke,39,40 depression,41,42 and in cancer survivors.43,44 Numerous systematic reviews have also reported that the efficacies of these common clinical ASRTs for primary insomnia and comorbid insomnia were higher than that of routine care, placebo acupuncture, or waiting list controls.45–53 However, the generalizability of these findings was constrained by the fact that the quality of the available literature is generally poor and these meta-analyses concentrated on a particular form of insomnia and/or a single therapy approach.
Each different ASRT has its own advantages and disadvantages. In clinical practice, the choice of ASRT is variable and flexible according to clinical experience or patient preference rather than a sound evidence base. Therefore, a thorough systematic review with strict inclusion criteria is required to shed light on the efficacy and safety of various common clinical ASRTs in patients with insomnia to inform clinical recommendations. Given the efficacy of ASRT depends on the choice of acupoints, the method of acupoint stimulation, and the pathophysiological condition of patients, this meta-analysis will: 1) assess the effectiveness of the most frequently used common clinical ASRTs including MA, EA, laser acupuncture, ACE, acupressure, moxibustion, and TEAS as monotherapies or adjuncts to recommended treatments (hypnotic drugs or CBT-I) for primary insomnia and comorbid insomnia; and 2) undertake subgroup analyses to detect potential ASRT effect confounders such as treatment features (eg, acupoint selection, stimulation technique, and treatment duration) and patient characteristics (eg, age, comorbidities, severity, and course of insomnia).
Materials and Methods
Study Registration
The Preferred Reporting Items for Systematic review and Meta-Analysis-Protocols (PRISMA-P) guidelines54 were followed in this protocol (Supplementary Table 1). Furthermore, the final review will be presented in accordance with PRISMA 2020 recommendations.55 This protocol has been registered on the International Platform of Registered Systematic Review and Meta-analysis (INPLASY) platform with a registration DOI of 10.37766/inplasy2021.12.0137.
Eligibility Criteria for Study Selection
Eligibility requirements will be determined in accordance with the review objectives and the PICOS (participants, intervention, comparison, outcome, and study design) method to guarantee a high-quality review.54
Type of Study Design
In this review, only full-text publications of RCTs evaluating common clinical ASRTs for the management of insomnia written in English and Chinese will be accepted. In cases where several publications present data for the same population, the most thorough report—the one with the greatest sample size, the longest follow-up, an exhaustive methods section, and an exhaustive results report—will be chosen.
Type of Participants
Participants with explicit evidence of insomnia symptoms by objective measurements or through standardized assessments like the Pittsburgh Sleep Quality Index (PSQI)56 or Athens Insomnia Scale (AIS);57 insomnia diagnosed using at least one of the internationally recognized classifications or equivalent standardized diagnostic criteria, such as the Diagnostic and Statistical Manual of Mental Disorders (DSM),58 International Classification of Sleep Disorders (ICSD),59 International Classification of Diseases (ICD),58 or Chinese Classification of Mental Disorders (CCMD);60 or with a complaint of insomnia symptoms will be included regardless of the type, reason, intensity, and length of insomnia as well as age, gender, nationality, occupation, and level of education. We will also include participants with co-existent physical or neuropsychiatric disorders, because participants with insomnia symptoms or insomnia disorder observed in clinical practice are likely to have co-morbid problems.
Types of Interventions
Only common clinical ASRTs (acupoints applied in accordance with TCM meridian theory) to treat or manage insomnia including MA, EA, laser acupuncture, ACE, acupressure, moxibustion, and TEAS will be evaluated.
Types of Comparisons
No treatment or waiting lists, routine care, placebo or sham treatments, or mainstream clinical insomnia therapies (hypnotic drugs or CBT-I) will be considered as control interventions. Five comparisons will be considered: (1) ASRT with no treatment or waiting lists; (2) ASRT with placebo or sham intervention; (3) ASRT with hypnotic drugs or CBT-I; (4) ASRT plus hypnotic drugs or CBT-I with hypnotic drugs or CBT-I alone; and (5) ASRT plus hypnotic drugs or CBT-I with a placebo or sham intervention plus hypnotic drugs or CBT-I.
Type of Outcome Measures
The primary outcome will be changes in sleep quality questionnaires or indices determined by standardized sleep scales such as the PSQI, the Insomnia Severity Index (ISI),61 the AIS,57 or the Leeds Sleep Evaluation Questionnaire (LSEQ).62 Additional outcomes will include: (1) objective sleep parameters, as determined by a sleep log or other sleep monitoring devices and techniques like actigraphy, electroencephalography, or polysomnography; (2) daytime function, as evaluated through performance tasks and self-reporting using standardized tests such as the Stanford Sleepiness Scale63 or Epworth Sleepiness Scale64 or through performance task assessments; (3) health-related quality of life (HRQoL), as assessed as a continuous variable using any validated global tools for evaluating functioning, such as the Short Form-36 (SF-36)65 or the WHO Quality of Life questionnaire;66 and (4) adverse events (AEs), with incidence of AEs observed in studies or evaluated using validated scales like the Treatment Emergent Symptom Scale (TESS) or Side Effects Rating Scale (SERS).
The exclusion criteria will be: (1) studies not reported in Chinese or English peer-reviewed journals; (2) studies without specific diagnostic criteria or outcome indicators; (3) studies with inadequate or missing data and repeat publications; (4) treatment did not focus on stimulated acupoints, or acupoints and locations stimulated were not based on TCM meridian theory; (5) RCTs that only compared different ASRTs or the combination of two or more ASRTs; (6) trials in which the sample size is unknown or the total sample size is <20. (7) studies published as non-RCTs such as retrospective studies, cohort studies, case reports, animal mechanism studies, reviews, commentaries, expert experience, and practice guidelines.
Information Sources and Search Strategy
The PubMed, Cochrane Central Register of Controlled Trials, Embase, Web of Science Core Collection, Chinese National Knowledge Infrastructure (CNKI), and Wanfang databases will be searched through a comprehensive search from inception to the search date. Medical subject headings (MeSH) and free-text terms associated with ASRTs, insomnia, and RCTs will be combined in the electronic databases to retrieve all possibly pertinent studies.
Prior to the search, any necessary revisions will be made to the keywords and subject terms for each database. No time restrictions will be applied; however, only English and Chinese publications will be included. In the event of disagreements, a decision will be achieved through discussion. As the examples illustrated, Supplementary Tables 2 and 3 detail the search strategy for PubMed and Embase electronic databases.
To obtain any additional eligible studies missed through automatic searching, the reference lists of the relevant systematic reviews and included studies will also be manually searched. Due to the substantial possibility for bias without peer review, we will not include grey literature. If there are disagreements, they will be discussed and resolved by consensus.
Article Selection
To locate all eligible clinical studies, two reviewers (PG and MMX) will separately but concurrently use EndNote X20 citation management software (Thomson Reuters, New York, NY) to remove duplicates and sequentially assess the study titles and abstracts for eligibility. For studies that cannot clearly be included based on the title and abstract, the full text will be carefully read to check for suitability for inclusion. For persistent disagreements about trial selection between the two reviewers, a final decision will be made through group discussion. Summary of the study selection process is shown in Figure 1.
 | Figure 1 Study selection procedure flow diagram. |
Data Extraction and Management
Two reviewers (PG and MMX) will independently extract the study details, study design, notes, participant characteristics, intervention and comparison characteristics, outcome data, and conclusions from the studies meeting the eligibility requirements. Data items are shown in Tables 1–4. In the event of a lack of consensus on data extraction and collection, a third reviewer (YG) will make the decision.
 | Table 1 Basic Characteristics of the Included RCTs |
 | Table 2 Summary of the Participant Characteristics |
 | Table 3 Summary of the Intervention/Comparison Characteristics |
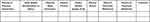 | Table 4 Summary of the Outcome Characteristics |
Risk of Bias Assessment
The Cochrane Collaboration's Risk of Bias (RoB) version 2.0 tool will be used by two independent reviewers (PG and MMX) to evaluate the RoB of each eligible RCT.67 RoB is evaluated across five domains (randomization, deviations from interventions, missing data, outcome measurement, result selection). Each domain will be given a bias rating of low risk, high risk, or unclear risk.67 Any questions or disagreement in the RoB assessment results between the reviewers will be resolved by consensus or adjudicated by a third reviewer (YG).
Dealing with Missing Data
We will contact appropriate authors or coauthors to ask about unclear data and/or request further details if the included data are insufficient or not supplied in the RCT reports. Studies will be disregarded if complete data cannot be obtained, and any potential impact of missing data on the findings will be evaluated in sensitivity analysis and discussed in the final review.
Data Analysis
Qualitative summaries of the included studies and results will be provided. A meta-analysis will be performed if more than three trials assess the same treatments and outcomes.68,69 To calculate the treatment effect, RevMan v5.4 software (Cochrane, London, UK) will be used to meta-analyze RCTs with sufficient data. Because the included RCTs are likely to comprise a wide range of intervention components, we will employ Mantel-Haenszel random-effects models for all meta-analyses. For continuous data, 95% confidence intervals (CIs) with a weighted mean difference (WMD) and a standard mean difference (SMD) will be calculated, whereas the risk ratio (RR) with 95% CIs will be used when analyzing dichotomous data. Two-sided tests will be used for all analyses, and a P-value <0.05 will be regarded as statistically significant.68 The evidence and results will be summarized in a written narrative if the data required for quantitative analysis are unavailable or insufficient.69 Using Cochrane's Q statistic and its associated P-value, statistical heterogeneity across RCTs will be evaluated. The I-squared statistic (I2 index), which ranges from 0–100%, will also be used as a measure to characterize heterogeneity between the included RCTs.68 An RCT will be deemed to have significant heterogeneity when the P-value is ≤0.1 and I2 index is ≥50%.68
Subgroup Analysis and Sensitivity Analysis
We will perform subgroup analyses for outcomes included in the RCTs when there are enough data to identify potential sources of heterogeneity in the following characteristics: publishing date, language, diagnostic criteria, characteristics of insomnia, presence or absence of co-morbidities, acupoint options, participant characteristics, intervention characteristics, comparison type, and level of RoB of included RCTs. After taking the impact of methodological quality, missing data, and sample size into account, sensitivity analyses will be performed on the results to explore the reliability and robustness of the review findings, when possible.
Reporting Bias Assessment
RevMan version 5.4 (Cochrane, London, UK) and STATA version 14.0 (Stata Corp., College Station, TX) statistical software will be applied to analyze reporting bias. Funnel plots70 will be used to identify potential reporting bias if over ten RCTs are obtained. The publication bias depicted in the funnel plot will be quantified using Begg's and Egger's tests.71
Confidence Assessments
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) guidelines will be used to evaluate the quality of evidence for each result. Evidence quality will be rated as very low, low, moderate, or high depending on the methodological quality of the included RCTs, study limitations, (in)consistency of results, (in)directness of evidence, imprecision, and publication bias.72
Ethical Considerations
Ethical approval and consent were not unnecessary since no data are related to patient information and privacy in this protocol.
Discussion
Insomnia, a highly prevalent clinical problem across the world, is frequently reported by patients and may be a significant sign of a number of sleep and medical illnesses. Indeed, epidemiological research has shown that the prevalence of insomnia among people of all ages is rising year on year.2,9 Insomnia places huge burdens on individuals, families, and society,2 but, despite this, insomnia has not received sufficient recognition nor management in clinical practice. An increasing number of clinical trials have reported that ASRTs guided by TCM theory are helpful for improving insomnia disorder and daytime functioning as well as being relatively cheap, convenient, available, and safe.29–37 ASRTs might represent a clinical treatment option that could be offered as a second-line treatment when first-line treatments are not viable or tolerated. In addition to acupuncture and acupressure, ASRTs have now evolved into numerous treatment techniques driven by clinical need, with acupoint selection varying from practitioner to practitioner. While several clinical common ASRTs for insomnia have been evaluated in previous systematic reviews,45–53 in the face of such a wide range of ASRTs, there is no conclusion on how ASRT clinicians should manage insomnia in clinical practice. To develop guidelines and further drive future clinical practice and research, a more thorough and comprehensive evaluation of all the existing literature is required. The clinically recognized acupoint stimulation techniques for the management of insomnia with or without comorbid physical or neuropsychiatric illnesses will be reviewed and assessed for efficacy and safety in this review. By doing this, we hope to provide answers to the issues of whether efficacy differs depending on the part of sleep being addressed as well as whether the effects vary depending on the precise acupoints used, the form of acupoint stimulation, or the type of insomnia present.
We believe that the study's many strengths will make its contributions meaningful. First, we will include all current common clinical ASRTs for insomnia reported in the "gold standard" of clinical trials – RCTs. Second, a wide search strategy will be applied to the present date to identify the largest number of available studies across a comprehensive set of databases in both English and Chinese. Third, the public, researchers, and clinicians should be able to rapidly evaluate the existing information and judge its quality thanks to the adoption of the publication bias and GRADE frameworks to assess the strength of the evidence.
Despite our careful methodological considerations, there might be some limitations to our review. First, excluding papers published in languages other than English and Chinese may omit some relevant studies. Also, the inclusion of only peer-reviewed studies may exclude grey literature containing relevant data and information; however, this will also ensure a minimum quality of included studies. The diverse ASRTs, insomnia patients' characteristics, insomnia severity, and RCT quality may introduce inevitable heterogeneity, so we plan to analyze all relevant factors in the future to explore sources of heterogeneity.
Conclusion
This review will expand on previous reviews through its up-to-date search of English and Chinese databases and obtaining the fullest scope of evidence. Moreover, our meta-analyses of RCTs will provide more accurate and quantitative insight into the efficacy and safety of common, clinically prescribed ASRTs for the management of insomnia. It will also provide valuable information about how common clinical ASRTs should be used to improve insomnia. The findings of this review will benefit patients, physicians, and decision makers working in healthcare to make informed decisions on evidence-based non-pharmacological interventions for insomnia disorder.
Abbreviations
ASRTs, Acupoint Stimulation-Related Therapies; TCM, Traditional Chinese Medicine; RCTs, Randomized Controlled Trials; GRADE, Grading of Recommendations, Assessment, Development and Evaluation; INPLASY, International Platform of Registered Systematic Review and Meta-analysis; GABA, Gamma-aminobutyric Acid; CBT-I, Cognitive Behavioral Therapy for Insomnia; MA, Manual Acupuncture; EA, Electro-acupuncture; PRISMA-P, Preferred Reporting Items for Systematic Review and Meta-analysis Protocols; PRISMA, Preferred Reporting Items for Systematic Review and Meta-Analysis; PICOS, Participants, Intervention, Comparison, Outcome, and Study Design; PSQI, Pittsburgh Sleep Quality Index; AIS, Athens Insomnia Scale; DSM, Diagnostic and Statistical Manual of Mental Disorders; ICSD, International Classification of Sleep Disorders; ICD, International Classification of Diseases; CCMD, Chinese Classification of Mental Disorders; WASO, Wake After Sleep Onset; ISI, Insomnia Severity Index; LSEQ, Leeds Sleep Evaluation Questionnaire; HRQoL, Health-related quality of life; SF-36, Short Form-36; AEs, Adverse events; TESS, Treatment Emergent Symptom Scale; SERS, Side Effects Rating Scale; CNKI, Chinese National Knowledge Infrastructure; MeSH, Medical Subject Headings, RevMan, Review Manager; RoB, Risk of bias; WMD, Weighted Mean Difference; SMD, Standard Mean Difference; Cis, Confidence Intervals; RR, Risk Ratio.
Author Contributions
All authors made a significant contribution to this work, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all of these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was supported by a grant from National Natural Science Foundation of China (grant number 82104983), Medical Scientific Program of Guangdong Province (grant number A2021071), Scientific Research Program by Traditional Chinese Medicine Bureau of Guangdong Province, China (grant number 20201103, 20231088), and Fundamental Research Funds for the Central Universities, China (grant number 21620362).
Disclosure
The authors have no conflicts of interest related to this work.
References
1. Buysse DJ. Insomnia. JAMA. 2013;309(7):706–716. doi:10.1001/jama.2013.193
2. Ferini-Strambi L, Auer R, Bjorvatn B, et al. Insomnia disorder: clinical and research challenges for the 21st century. Eur J Neurol. 2021;28(7):2156–2167. doi:10.1111/ene.14784
3. Perlis ML, Posner D, Riemann D, Bastien CH, Teel J, Thase M. Insomnia. Lancet. 2022;400(10357):1047–1060. doi:10.1016/S0140-6736(22)00879-0
4. Morin CM, Drake CL, Harvey AG, et al. Insomnia disorder. Nat Rev Dis Primers. 2015;1:15026. doi:10.1038/nrdp.2015.26
5. Sutton EL. Insomnia. Ann Intern Med. 2021;174(3):ITC33–ITC48. doi:10.7326/AITC202103160
6. Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. doi:10.1053/smrv.2002.0186
7. Chung KF, Yeung WF, Ho FY, et al. Cross-cultural and comparative epidemiology of insomnia: the Diagnostic and statistical manual (DSM), International classification of diseases (ICD) and International classification of sleep disorders (ICSD). Sleep Med. 2015;16(4):477–482. doi:10.1016/j.sleep.2014.10.018
8. Cao XL, Wang SB, Zhong BL, et al. The prevalence of insomnia in the general population in China: a meta-analysis. PLoS One. 2017;12(2):e0170772. doi:10.1371/journal.pone.0170772
9. Kocevska D, Lysen TS, Dotinga A, et al. Sleep characteristics across the lifespan in 1.1 million people from the Netherlands, United Kingdom and United States: a systematic review and meta-analysis. Nat Hum Behav. 2021;5(1):113–122. doi:10.1038/s41562-020-00965-x
10. de Zambotti M, Goldstone A, Colrain IM, et al. Insomnia disorder in adolescence: diagnosis, impact, and treatment. Sleep Med Rev. 2018;39:12–24. doi:10.1016/j.smrv.2017.06.009
11. Anothaisintawee T, Reutrakul S, Van Cauter E, et al. Sleep disturbances compared to traditional risk factors for diabetes development: systematic review and meta-analysis. Sleep Med Rev. 2016;30:11–24. doi:10.1016/j.smrv.2015.10.002
12. Ferini-Strambi L, Galbiati A, Casoni F, et al. Therapy for insomnia and circadian rhythm disorder in alzheimer disease. Curr Treat Options Neurol. 2020;22(2):4. doi:10.1007/s11940-020-0612-z
13. Pigeon WR, Bishop TM, Krueger KM. Insomnia as a precipitating factor in new onset mental illness: a systematic review of recent findings. Curr Psychiatry Rep. 2017;19(8):44. doi:10.1007/s11920-017-0802-x
14. Hertenstein E, Feige B, Gmeiner T, et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. 2019;43:96–105. doi:10.1016/j.smrv.2018.10.006
15. He Q, Zhang P, Li G, et al. The association between insomnia symptoms and risk of cardio cerebral vascular events: a meta-analysis of prospective cohort studies. Eur J Prev Cardiol. 2017;24(10):1071–1082. doi:10.1177/2047487317702043
16. Javaheri S, Redline S. Insomnia and risk of cardiovascular disease. Chest. 2017;152(2):435–444. doi:10.1016/j.chest.2017.01.026
17. Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73(9):e1160–e1167. doi:10.4088/JCP.11r07586
18. Palagini L, Cipollone G, Masci I, et al. Insomnia symptoms predict emotional dysregulation, impulsivity and suicidality in depressive bipolar II patients with mixed features. Compr Psychiatry. 2019;89:46–51. doi:10.1016/j.comppsych.2018.12.009
19. Riemann D, Nissen C, Palagini L, et al. The neurobiology, investigation, and treatment of chronic insomnia. Lancet Neurol. 2015;14(5):547–558. doi:10.1016/S1474-4422(15
20. Kay-Stacey M, Attarian H. Advances in the management of chronic insomnia. BMJ. 2016;354:i2123. doi:10.1136/bmj.i2123
21. Qaseem A, Kansagara D, Forciea MA, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American college of physicians. Ann Intern Med. 2016;165(2):125–133. doi:10.7326/M15-2175
22. Wilt TJ, MacDonald R, Brasure M, et al. Pharmacologic treatment of insomnia disorder: an evidence report for a clinical practice guideline by the American college of physicians. Ann Intern Med. 2016;165(2):103–112. doi:10.7326/M15-1781
23. Everitt H, Baldwin DS, Stuart B, et al. Antidepressants for insomnia in adults. Cochrane Database Syst Rev. 2018;5:CD010753. doi:10.1002/14651858.CD010753.pub2
24. Kuriyama A, Tabata H. Suvorexant for the treatment of primary insomnia: a systematic review and meta-analysis. Sleep Med Rev. 2017;35:1–7. doi:10.1016/j.smrv.2016.09.004
25. Trauer JM, Qian MY, Doyle JS, et al. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med. 2015;163(3):191–204. doi:10.7326/M14-2841
26. Edinger JD, Arnedt JT, Bertisch SM, et al. Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2021;17(2):255–262. doi:10.5664/jcsm.8986
27. Koffel E, Bramoweth AD, Ulmer CS. Increasing access to and utilization of cognitive behavioral therapy for insomnia (CBT-I): a narrative review. J Gen Intern Med. 2018;33(6):955–962. doi:10.1007/s11606-018-4390-1
28. Espie CA, Inglis SJ, Tessier S, et al. The clinical effectiveness of cognitive behaviour therapy for chronic insomnia: implementation and evaluation of a sleep clinic in general medical practice. Behav Res Ther. 2001;39(1):45–60. doi:10.1016/s0005-7967(99
29. Wang C, Xu WL, Li GW, et al. Impact of acupuncture on sleep and comorbid symptoms for chronic insomnia: a randomized clinical trial. Nat Sci Sleep. 2021;13:1807–1822. doi:10.2147/NSS.S326762
30. Zhang L, Tang Y, Hui R, et al. The effects of active acupuncture and placebo acupuncture on insomnia patients: a randomized controlled trial. Psychol Health Med. 2020;25(10):1201–1215. doi:10.1080/13548506.2020.1738015
31. Lee B, Kim BK, Kim HJ, et al. Efficacy and safety of electroacupuncture for insomnia disorder: a multicenter, randomized, assessor-blinded, controlled trial. Nat Sci Sleep. 2020;12:1145–1159. doi:10.2147/NSS.S281231
32. Yeung WF, Yu BY, Yuen JW, et al. Semi-Individualized Acupuncture for Insomnia Disorder and Oxidative Stress: a Randomized, Double-Blind, Sham-Controlled Trial. Nat Sci Sleep. 2021;13:1195–1207. doi:10.2147/NSS.S318874
33. Chen CK, Lin YC, Cheng JW, et al. Effectiveness of laser acupuncture in alleviating chronic insomnia: a single-blinded randomized controlled trial. Evid Based Complement Alternat Med. 2019;2019:8136967. doi:10.1155/2019/8136967
34. Xu F, Xuan LH, Zhou HJ, et al. Acupoint catgut embedding alleviates insomnia in different Chinese medicine syndrome types: a randomized controlled trial. Chin J Integr Med. 2019;25(7):543–549. doi:10.1007/s11655-018-2770-3
35. Yeung WF, Yu BY, Chung KF, et al. Self-administered acupressure for insomnia disorder: a randomized controlled trial. Phytomedicine. 2022;99:153993. doi:10.1016/j.phymed.2022.153993
36. Chen Y, Gao X, Sun C. Pricking and penetrating moxibustion therapy in patients with refractory insomnia: a randomized and controlled clinical trial. J Tradit Chin Med. 2018;38(5):754–762. doi:10.1016/S0254-6272(18)30915-4
37. Song B, Chang Y, Li Y, Zhu J. Effects of transcutaneous electrical acupoint stimulation on the postoperative sleep quality and pain of patients after video-assisted thoracoscopic surgery: a prospective, randomized controlled trial. Nat Sci Sleep. 2020;12:809–819. doi:10.2147/NSS.S270739
38. Foroughinia S, Hessami K, Asadi N, et al. Effect of acupuncture on pregnancy-related insomnia and melatonin: a single-blinded, randomized, placebo-controlled trial. Nat Sci Sleep. 2020;12:271–278. doi:10.2147/NSS.S247628
39. Cao Y, Yan YJ, Xu JY, et al. Acupuncture for insomnia after ischemic stroke: an assessor-participant blinded, randomized controlled trial. Acupunct Med. 2022;40(5):443–452. doi:10.1177/09645284221077106
40. Song Y, Wang X, Schubert F. Application of wireless dynamic sleep monitor in acupuncture treatment of insomnia after ischemic stroke: a retrospective study. Evid Based Complement Alternat Med. 2021;2021:5524622. doi:10.1155/2021/5524622
41. Yin X, Li W, Wu H, et al. Efficacy of electroacupuncture on treating depression-related insomnia: a randomized controlled trial. Nat Sci Sleep. 2020;12:497–508. doi:10.2147/NSS.S253320
42. Yin X, Li W, Liang T, et al. Effect of electroacupuncture on insomnia in patients with depression: a randomized clinical trial. JAMA Netw Open. 2022;5(7):e2220563. doi:10.1001/jamanetworkopen.2022.20563
43. Garland SN, Xie SX, DuHamel K, et al. Acupuncture versus cognitive behavioral therapy for insomnia in cancer survivors: a randomized clinical trial. J Natl Cancer Inst. 2019;111(12):1323–1331. doi:10.1093/jnci/djz050
44. Lee B, Kim BK, Kim M, et al. Electroacupuncture for treating cancer-related insomnia: a multicenter, assessor-blinded, randomized controlled, pilot clinical trial. BMC Complement Med Ther. 2022;22(1):77. doi:10.1186/s12906-022-03561-w
45. Cheuk DK, Yeung WF, Chung KF, Wong V. Acupuncture for insomnia. Cochrane Database Syst Rev. 2012;(9):CD005472. doi:10.1002/14651858.CD005472
46. Zhao FY, Fu QQ, Kennedy GA, et al. Can acupuncture improve objective sleep indices in patients with primary insomnia? A systematic review and meta-analysis. Sleep Med. 2021;80:244–259. doi:10.1016/j.sleep.2021.01.053
47. Liu FG, Tan AH, Peng CQ, Tan YX, Yao MC. Efficacy and safety of scalp acupuncture for insomnia: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2021;2021:6621993. doi:10.1155/2021/6621993
48. Jing R, Feng K. Efficacy of intradermal acupuncture for insomnia: a meta-analysis. Sleep Med. 2021;85:66–74. doi:10.1016/j.sleep.2021.06.034
49. Zhang J, He Y, Huang X, Liu Y, Yu H. The effects of acupuncture versus sham/placebo acupuncture for insomnia: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Clin Pract. 2020;41:101253. doi:10.1016/j.ctcp.2020.101253
50. Zhang J, Zhang Z, Huang S, et al. Acupuncture for cancer-related insomnia: a systematic review and meta-analysis. Phytomedicine. 2022;102:154160. doi:10.1016/j.phymed.2022.154160
51. Yu H, Liu C, Chen B, et al. The clinical efficacy and safety of acupuncture intervention on cancer-related insomnia: a systematic review and meta-analysis. Front Neurosci. 2022;16:1026759. doi:10.3389/fnins.2022.1026759
52. Zhou L, Hu X, Yu Z, et al. Efficacy and safety of acupuncture in the treatment of poststroke insomnia: a systematic review and meta-analysis of twenty-six randomized controlled trials. Evid Based Complement Alternat Med. 2022;2022:5188311. doi:10.1155/2022/5188311
53. Zhao FY, Kennedy GA, Spencer SJ, et al. The role of acupuncture in the management of insomnia as a major or residual symptom among patients with active or previous depression: a systematic review and meta-analysis. Front Psychiatry. 2022;13:863134. doi:10.3389/fpsyt.2022.863134
54. Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. doi:10.1136/bmj.g7647
55. Yepes-Nuñez JJ, Urrútia G, Romero-García M, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Rev Esp Cardiol. 2021;74(9):790–799. doi:10.1016/j.rec.2021.07.010
56. Mollayeva T, Thurairajah P, Burton K, et al. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med Rev. 2016;25:52–73. doi:10.1016/j.smrv.2015.01.009
57. Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. 2000;48(6):555–560. doi:10.1016/s0022-3999(00)00095-7
58. Biedermann F, Fleischhacker WW. Psychotic disorders in DSM-5 and ICD-11. CNS Spectr. 2016;21(4):349–354. doi:10.1017/S1092852916000316
59. Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387–1394. doi:10.1378/chest.14-0970
60. Chen Y-F. Chinese classification of mental disorders (CCMD-3): towards integration in international classification. Psychopathology. 2002;35(2–3):171–175. doi:10.1159/000065140
61. Morin CM, Belleville G, Bélanger L, et al. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi:10.1093/sleep/34.5.601
62. Parrott AC, Hindmarch I. The leeds sleep evaluation questionnaire in psychopharmacological investigations - a review. Psychopharmacology. 1980;71(2):173–179. doi:10.1007/BF00434408
63. Maclean AW, Fekken GC, Saskin P, Knowles JB. Psychometric evaluation of the Stanford Sleepiness Scale. J Sleep Res. 1992;1(1):35–39. doi:10.1111/j.1365-2869.1992.tb00006.x
64. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi:10.1093/sleep/14.6.540
65. Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305(6846):160–164. doi:10.1136/bmj.305.6846.160
66. Whoqol G. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28(3):551–558. doi:10.1017/s0033291798006667
67. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi:10.1136/bmj.l4898
68. Siddaway AP, Wood AM, Hedges LV. How to do a systematic review: a best practice guide for conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annu Rev Psychol. 2019;70:747–770. doi:10.1146/annurev-psych-010418-102803
69. Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10:ED000142. doi:10.1002/14651858.ED000142
70. Peters JL, Sutton AJ, Jones DR, et al. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol. 2008;61(10):991–996. doi:10.1016/j.jclinepi.2007.11.010
71. Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53(11):1119–1129. doi:10.1016/s0895-4356(00)00242-0
72. Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi:10.1136/bmj.39489.470347.AD

Comments
Post a Comment