2022 ACC/AHA Guideline for the Diagnosis and Management of ...
Mitral Valve Replacement Gets A Favorable Match-Up Against GDMT In Functional MR
PARIS -- Transcatheter mitral valve replacement (TMVR) could be the better choice over conservative therapy for secondary (or functional) mitral regurgitation (MR), according to researchers settling for an indirect retrospective comparison in the face of absent randomized data.
People who received investigational TMVR devices as part of the CHOICE-MI registry were propensity-matched with peers from the guideline-directed medical therapy (GDMT) arm of COAPT, the controls of a trial originally designed to test another technology, transcatheter edge-to-edge repair (TEER).
Based on 97 matched pairs, 2-year clinical outcomes largely favored the TMVR cohort, according to Sebastian Ludwig, MD, of University Heart and Vascular Center Hamburg, Germany:
Ludwig presented his group's findings at the EuroPCR conference and had the full study manuscript published simultaneously in Circulation: Cardiovascular Interventions.
"In the absence of randomized controlled trials, these results provide important preliminary evidence on the benefits of TMVR," he said.
He cautioned, however, that this was an exploratory analysis that featured highly selected populations and was not powered to detect a difference in survival. His report also left room for selection bias given the likelihood of unaccounted-for anatomical differences between TMVR and GDMT groups. Echocardiographic follow-up was also incomplete.
Secondary MR differs from primary MR in that it is related to left ventricular dysfunction instead of abnormalities in the mitral valve leaflets and chords themselves.
Patients with secondary MR showed clinical benefits from MitraClip TEER in the COAPT trial. Nevertheless, mere clipping may not be enough for this MR subtype, as suggested by a separate real-world analysis by Ludwig's group in which TMVR was associated with better secondary MR reduction and superior symptom improvement (notwithstanding an early disadvantage in survival) compared with TEER.
During a press conference, Ludwig said more definitive randomized data are absent primarily due to a high rate of screening failure that has resulted in early feasibility trials of TMVR being slow to enroll.
CHOICE-MI is a retrospective registry that includes patients screened for TMVR regardless of ultimate treatment. Participants received a variety of dedicated devices, albeit mostly transapical ones (i.E., the Tendyne bioprosthetic valve), according to Ludwig.
He suggested that a transfemoral system may produce better results, particularly when it comes to TMVR's lackluster mortality data, currently the "elephant in the room."
Yet the reduction in heart failure hospitalization is in itself a "huge" achievement by TMVR as this was not seen in the surgical literature, according to session panelist Patrizio Lancellotti, MD, PhD, of University of Liège, Belgium.
And there is more room for hope as operators move away from transapical approaches, suggested fellow panelist Ralph Stephan von Bardeleben, MD, PhD, of Universitätsmedizin der Johannes Gutenberg-Universität Mainz, Germany. The later experience with TMVR may also improve, as CHOICE captured the first compassionate use cases, von Bardeleben said.
He concluded that the present study marks an "important step," as it shows there's "at least no disadvantage" but instead a possible advantage in clinical outcomes after TMVR for secondary MR.
Nicole Lou is a reporter for MedPage Today, where she covers cardiology news and other developments in medicine. Follow
Disclosures
Ludwig disclosed relationships with the German Heart Foundation, Edwards Lifesciences, Abbott, and Bayer.
Lancellotti had no disclosures.
Von Bardeleben reported research support from Abbott.
Primary Source
EuroPCR
Source Reference: Ludwig S "Outcomes of TMVR vs. Medical therapy for secondary mitral regurgitation: A propensity score matched analysis" EuroPCR 2023.
Secondary Source
Circulation: Cardiovascular Interventions
Source Reference: Ludwig S, et al "Transcatheter mitral valve replacement versus medical therapy for secondary mitral regurgitation: A propensity score-matched comparison" Circ Cardiovasc Interv 2023; DOI: 10.1161/CIRCINTERVENTIONS.123.013045.
Please enable JavaScript to view the comments
MITRAL At 5 Years: TMVR For MAC, Failing Devices Shows Ongoing Impact
PARIS, France—Final, 5-year results of the MITRAL trial continue to support transcatheter mitral valve replacement (TMVR) in patients with failing bioprostheses or prosthetic rings, and with mitral annular calcification (MAC).
MITRAL was the first study to prospectively evaluate the safety and feasibility of mitral valve-in-valve (ViV), valve-in-ring (ViR), and valve-in-mitral annular calcification (ViMAC) procedures, using devices first approved for aortic stenosis. Initial 30-day results, released in 2017 at the TCT and American Heart Association annual meetings, were promising.
Here at EuroPCR 2023, Mayra Guerrero, MD (Mayo Clinic, Rochester, MN), summed up the full findings by saying that these TMVR procedures are "a reasonable alternative for patients who have high surgical risk and favorable anatomy." This is important, she added, as "redo mitral surgery and surgery in severe MAC are often associated with high risk."
For the MITRAL study, Guerrero and colleagues enrolled 91 patients at extremely high surgical risk who had severe mitral stenosis (mitral valve area ≤ 1.5 cm2) after a failed bioprosthetic valve (n = 30), after a failed surgical ring (n = 30), or with native MAC (n = 31). All underwent TMVR using a Sapien XT or Sapien 3 valve (Edwards Lifesciences).
Most of the ViV and ViMAC patients were female (63.3% and 71.0%, respectively), whereas 36.7% of the ViR group were female. Mean age ranged from 71.7 in the ViR patients up to 76.4 in the ViV patients, while mean STS scores were 8.6 for ViMAC, 8.7 for ViR, and 10.2 for ViV. The pathology for ViV and ViMAC was mostly stenosis (73.3% and 74.2%, respectively), whereas in the ViR group it was mostly regurgitation (56.7%)
Patients were assessed at 30 days and then annually thereafter through 5 years.
By 5-year follow-up, ViV patients had the lowest rates of death, mitral valve reintervention, and hemolytic anemia compared with the other two groups. "However, transcatheter valve thrombosis and endocarditis events were very low," Guerrero pointed out.
MITRAL Trial: Outcomes at 5 Years
ViV
(n = 28)
ViR
(n = 29)
ViMAC
(n = 28)
All-Cause Death
21.4%
65.5%
67.9%
Mitral Valve Reintervention
3.6%
10.3%
17.9%
Hemolytic Anemia
0
6.9%
17.9%
Transcatheter Valve Thrombosis
3.6%
0
7.1%
Valve Endocarditis
0
0
7.1%
"Mean gradients remained stable," at 6.6 mm Hg in ViV, 5.8 mm Hg in ViR, and 6.7 mm Hg in ViMAC, ViR, and ViMAC, said Guerrero, and "the vast majority had 1+ or less residual mitral regurgitation at 5 years." Fully 100% of the surviving ViV and ViMAC patients had levels considered mild or no/trace, as did two-thirds of the ViR survivors.
"We found significant improvement in heart failure symptoms and quality of life scores, which were sustained at 5 years," she told EuroPCR attendees. At baseline, 81% had been in NYHA class III/IV, but by 5-year follow-up, 75% were in NYHA class I/II. There also was an overall increase in median Kansas City Cardiomyopathy Questionnaire score. Looking at the three groups separately, the ViV patients saw the largest gains for both metrics.
Why Such Disparate Results?
Session moderator Fabien Praz, MD (Bern University Hospital, Switzerland), opened the discussion following Guerrero's presentation by highlighting the "huge differences in mortality between the strategies."
Simon Redwood, MD (St. Thomas' Hospital, London, England), the discussant after Guerrero's presentation, also said the discrepancy took him by surprise. "I can understand the difference in outcomes between valve-in-valve and valve-in-MAC, but what really strikes me is the outcomes of valve-in-ring are as bad as valve-in-MAC. I was trying to get my head around: why is that? Is that because their baseline ejection fraction is less? Is it because they present more with regurgitation? Are we putting valves in incomplete rings? Are we doing the procedures too late in the time course of their disease? I don't know. What do you think?"
In reply, Guerrero said, "You just answered the question, I think. [It's] because of all those reasons. I think these patients are different, absolutely different."
Although they carefully selected patients, it turned out that one or two of the rings they treated were rigid, making them "not favorable" for TMVR. "They can have increased gradients or significant residual regurgitation, and we know that leaving MR behind is not good," she explained.
Techniques have improved over time, added Guerrero, a point she elaborated on to TCTMD.
A decade ago, when she and her team did their first case in August 2013, "we did not know what we know now," Guerrero continued. Over the years they learned that LV outflow tract (LVOT) obstruction is a strong predictor of mortality and that preemptive alcohol ablation can be protective. "All those learnings have been applied now by others in other trials," she said.
All that knowledge has gone into the careful design of MITRAL II, for which Guerrero is principal investigator. The study is comparing patients treated with transseptal ViMAC versus controls who receive medical treatment (and who can't undergo the intervention due to anatomical or other exclusion criteria). In the ViMAC arm, the study is allowing preemptive alcohol septal ablation, preemptive radiofrequency septal ablation, or percutaneous laceration of the anterior leaflet to reduce the risk of TMVR-induced LVOT obstruction.
"The trial is enrolling rapidly and we hope to be done with enrollment later this year," said Guerrero.
As for the original, 5-year MITRAL results, panelist Patrizio Lancellotti, PhD (University of Liège, Belgium), pointed out that the long-term data are notable for the low rate of thrombosis and infective endocarditis. "This is huge. This is very important to mention, and it should be clearly emphasized," he stressed.
Guerrero agreed, noting that the performance of the valve and stable gradients are also positive findings.
Heart Valve Disorders
Heart valve disorders can affect any of the valves in your heart. The cause can be a leakage of blood (regurgitation), a narrowing of the valve opening (stenosis), or a combination of the two.
Some people with a heart valve disorder may not have any symptoms. But if it goes untreated, it can cause heart failure with worsening symptoms over time. Depending on how low your heart functioning is, this can lead to deadly ventricular arrhythmia.
Read on to learn more about how heart valves work, how disorders can develop, what can cause them, and what the treatments are.
Your heart valves open and close with each heartbeat, allowing blood to flow through the atria (upper chambers) and ventricles (lower chambers).
Your heart has these four valves:
Blood flows from the right and left atria through the tricuspid and mitral valves, which open to allow blood to flow into the right and left ventricles. These valves then close to prevent blood from flowing back into the atria.
Once the ventricles have filled with blood, they begin to contract, forcing the pulmonary and aortic valves to open. Blood then flows to the pulmonary artery and aorta. The pulmonary artery carries deoxygenated blood from the heart to the lungs. The aorta, which is the body's largest artery, carries oxygen-rich blood to the rest of your body.
The heart valves work by ensuring that blood flows in a forward direction and doesn't back up or cause leakage. If you have a heart valve disorder, the valve isn't able to do this job properly.
Learn more about the anatomy of the heart.
The following are the different types of heart valve disorders that may develop:
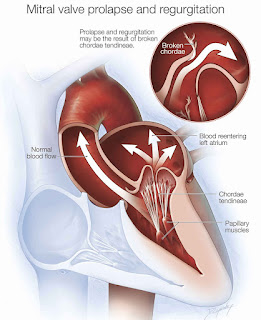
Mitral valve prolapseA mitral valve prolapse is also called:
It occurs when the mitral valve doesn't close properly, sometimes causing blood to flow back into the left atrium. Treatment involves surgery to repair or replace the mitral valve. Mitral valve prolapse occurs in about 2%-4% of people in high-income countries.
Bicuspid aortic valve diseaseBicuspid aortic valve disease occurs when a person is born with an aortic valve that has two flaps instead of the usual three. In very severe cases, the symptoms of this type of disorder are present at birth.
However, some people may go decades without knowing they have this type of disorder. It affects about 0.5% to 1.4% of the population.
The valve is usually able to function for years without causing symptoms, so most people with bicuspid aortic valve disease aren't diagnosed until adulthood. Most people are able to have their aortic valve repaired successfully with surgery.
Valvular stenosisValvular stenosis occurs when a valve isn't able to open completely, which means that not enough blood can flow through the valve. This can occur in any of the heart valves and may be caused by the heart valve thickening or stiffening.
About 0.3% to 0.5% of people are diagnosed with valvular stenosis, with the prevalence rising to 2%-7% among those over 65.
Some people don't need treatment for valvular stenosis. Other people may need surgery to replace or repair the valve. Depending on the severity of your stenosis and your age, valvuloplasty, which uses a balloon to dilate the valve, may be an option.
Valvular regurgitationValvular regurgitation may also be called a "leaky valve." It can also be referred to as mitral or tricuspid regurgitation. It occurs when any of the heart valves don't close properly, causing blood to flow backward. This occurs in about 0.9% of Americans of both sexes each year.
The effects of valvular regurgitation vary depending on the person. Some people simply need to have their condition monitored. Others may need to have medication to prevent fluid buildup, while others require valve repair or replacement.
Symptoms of heart valve disorders vary depending on the severity of the disorder. Usually, the presence of symptoms indicates that the disorder is affecting blood flow.
Many individuals with mild or moderate heart valve disorders don't experience any symptoms. However, signs and symptoms may include:
There are a number of causes for the different heart valve disorders. The causes may include:
If you're experiencing symptoms of a heart valve disorder, your doctor will begin by listening to your heart with a stethoscope. They'll listen for any heart rate abnormalities that might indicate a problem with your heart valves.
Your doctor may also listen to your lungs to determine if there's fluid buildup and check your body for signs of water retention. These are both signs of heart valve problems.
Other tests that may be used to diagnose heart valve disorders include the following:
Treatments for heart valve disorders depend on the severity of the disorder and its symptoms. Most doctors suggest beginning with conservative treatments. These include:
Medications that are usually prescribed are:
You may need surgery if your symptoms increase in severity. This may include a heart valve repair using one of the following:
Valvuloplasty may also be used to treat stenosis. During valvuloplasty, your doctor inserts a small balloon into your heart, where it's inflated slightly. The inflation increases the size of the opening in the valve, and then the balloon is removed.
Another less invasive option is transcatheter aortic valve replacement (TAVR), in which the surgeon replaces the narrowed or blocked heart valve through a catheter.
Your outlook will depend on what heart valve disorder you have and how severe it is. Some heart valve disorders only require routine monitoring, while others require surgery.
However, in cases of severe disease, corrective surgery can have a major impact on your outlook. Only 40%-60% of people with severe symptomatic aortic valve disease who don't get surgery survive to 3 years after diagnosis. However, 80%-90% of those who do get a valve replacement survive for the same period of time.
Talk with your doctor about any symptoms you have that you're concerned about, and make sure you schedule routine checkups with your doctor. This will make it more likely that your doctor will discover any potentially serious conditions in the early stages.

Comments
Post a Comment